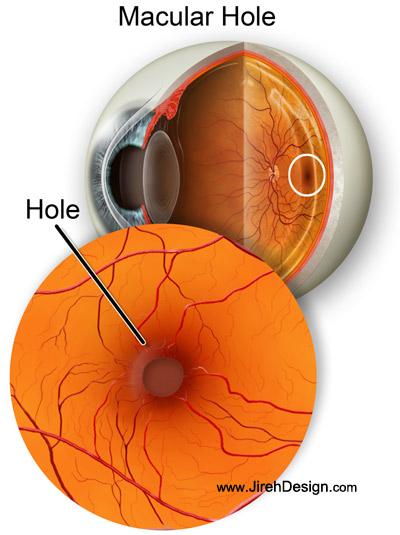
Macular hole
An illustrated guide to macular hole, causes, treatments and surgery descriptions Also see “Human Eye” animation What is a macular … Continue reading Macular hole


Macular hole
An illustrated guide to macular hole, causes, treatments and surgery descriptions Also see “Human Eye” animation What is a macular … Continue reading Macular hole
An illustrated guide to macular hole, causes, treatments and surgery descriptions
Also see “Human Eye” animation
What is a macular hole?
A macular hole is a small break in the macula, located in the center of the eye’s light-sensitive tissue, called the retina. The macula provides the sharp, central vision we need for reading, driving, and seeing fine detail. A macular hole can cause blurry and distorted central vision. Macular holes occur more with aging, usually in people over age 60.
Is a macular hole the same as age-related macular degeneration?
No. Macular holes and age-related macular degeneration are two separate and distinct eye conditions, although the symptoms for each are similar. Both conditions are common in people 60 and over. Your eye doctor will know the difference.
What causes a macular hole?
Most of the eye’s interior is filled with vitreous, a gel-like substance that fills about 80 percent of the eye and helps it maintain a round shape. The vitreous contains millions of fine fibers that are attached to the surface of the retina. As we age, the vitreous slowly shrinks and pulls away from the retinal surface. Natural fluids fill the area where the vitreous has contracted. This is normal and is called a vitreous detachment.
VIDEO footage of Vitreous Detachment
In most cases, there are no adverse effects. Some patients may experience a small increase in floaters, which are little “cobwebs” or specks that seem to float about in your field of vision.
However, if the vitreous is firmly attached to the retina when it pulls away, it can tear the retina and create a macular hole. Also, once the vitreous pulls away from the surface of the retina, some of the fibers can remain on the retinal surface and can contract. This increases tension on the retina and can lead to a macular hole. In either case, the fluid that displaces the shrunken vitreous can then seep through the hole onto the macula, blurring and distorting central vision.
Macular holes can also occur as a complication of eye disorders, such as high myopia (nearsightedness), macular pucker, and retinal detachment; eye disease, such diabetic retinopathy and Best’s disease; and injury to the eye.
What are the symptoms of a macular hole?
Macular holes often begin gradually. In the early stage of a macular hole, people may notice a slight distortion or blurriness in their straight-ahead vision. Straight lines or objects can begin to look bent or wavy. Reading and performing other routine tasks with the affected eye become difficult.
Are there different types of a macular hole?
Yes. There are three stages to a macular hole:
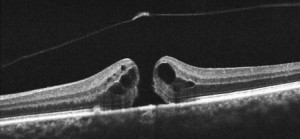
- Foveal detachments (Stage I). Without treatment, about half of Stage I macular holes will progress.
- Partial-thickness holes (Stage II). Without treatment, about 70 percent of Stage II macular holes will progress.
- Full-thickness holes (Stage III).
The size of the hole and its location on the retina determine how much it will affect a person’s visual acuity. When a Stage III macular hole develops, most central and detailed vision can be lost. If left untreated, a macular hole can lead to a detached retina, a sight-threatening condition that should receive immediate medical attention.
How do you treat a macular hole?

Following surgery, patients must remain in a face-down position, normally for a day or two but sometimes for as long as two-to-three weeks. This position allows the bubble to press against the macula and be gradually reabsorbed by the eye, sealing the hole. As the bubble is reabsorbed, the vitreous cavity refills with natural eye fluids.
Maintaining a face-down position is crucial to the success of the surgery. Because this position can be difficult for many people, it is important to discuss this with your doctor before surgery.
What are the risks of surgery?
The most common risk following macular hole surgery is an increase in the rate of cataract development. In most patients, a cataract can progress rapidly, and often becomes severe enough to require removal. Other less common complications include infection and retinal detachment either during surgery or afterward, both of which can be immediately treated.
For a few months after surgery, patients are not permitted to travel by air. Changes in air pressure may cause the bubble in the eye to expand, increasing pressure inside the eye.
How successful is this surgery?
Vision improvement varies from patient to patient. People that have had a macular hole for less than six months have a better chance of recovering vision than those who have had one for a longer period. Discuss vision recovery with your doctor before your surgery. Vision recovery can continue for as long as three months after surgery.
What if I cannot remain in a face-down position after the surgery?
If you cannot remain in a face-down position for the required period after surgery, vision recovery may not be successful. People who are unable to remain in a face-down position for this length of time may not be good candidates for a vitrectomy. However, there are a number of devices that can make the “face-down” recovery period easier on you. There are also some approaches that can decrease the amount of “face-down” time. Discuss these with your doctor.
Is my other eye at risk?
If a macular hole exists in one eye, there is a 10-15 percent chance that a macular hole will develop in your other eye over your lifetime. Your doctor can discuss this with you.
Other Resources
The following organization may be able to provide additional information on macular holes:
American Academy of Ophthalmology
P.O. Box 7424
San Francisco, CA 94120-7424
(415) 561-8500
Distributes a fact sheet on macular hole for patients.
Some information courtesy of the National Eye Institute