All about glaucoma
All about glaucoma
Glaucoma is a group of diseases that can damage the eye, resulting in vision loss. Here, you can read all about glaucoma.
Glaucoma can damage the optic nerve on the back of the eye. However, with early treatment, you can often protect your eyes against serious vision loss.
All about glaucoma and the optic nerve?
Also see a “Human Eye” animation
The optic nerve is a bundle of more than 1 million nerve fibers. It connects the retina to the brain. The retina is the light-sensitive tissue at the back of the eye. A healthy optic nerve is necessary for good vision.
How does open-angle glaucoma damage the optic nerve?
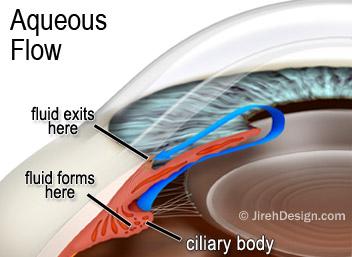
In the front of the eye is a space called the anterior chamber. A clear fluid flows continuously in and out of the chamber and nourishes nearby tissues. The fluid leaves the chamber at the open angle where the cornea and iris meet. When the fluid reaches the angle, it flows through a spongy meshwork, like a drain, and leaves the eye.
Sometimes, when the fluid reaches the angle, it passes too slowly through the meshwork drain. As the fluid builds up, the pressure inside the eye rises to a level that may damage the optic nerve. When the optic nerve is damaged from increased pressure, open-angle glaucoma–and vision loss–may result. That’s why controlling pressure inside the eye is important.
Does increased eye pressure mean that I have glaucoma?
Not necessarily. Increased eye pressure means you are at risk for glaucoma, but does not mean you have the disease. A person has glaucoma only if the optic nerve is damaged. If you have increased eye pressure but no damage to the optic nerve, you do not have glaucoma. However, you are at risk. Follow the advice of your eye care professional.
I’ve read all about glaucoma because my doctor says I have it. But I don’t have increased eye pressure?
Not every person with increased eye pressure will develop glaucoma. Some people can tolerate higher eye pressure better than others. Also, a certain level of eye pressure may be high for one person but normal for another.
Whether you develop glaucoma depends on the level of pressure your optic nerve can tolerate without being damaged. This level is different for each person. That’s why a comprehensive dilated eye exam is very important. It can help your eye care professional determine what level of eye pressure is normal for you.
Glaucoma can develop without increased eye pressure. This form of glaucoma is called low-tension or normal-tension glaucoma. It is not as common as open-angle glaucoma.
Who is at risk for open-angle glaucoma?
Anyone can develop glaucoma. Some people are at higher risk than others. They include:
African Americans over age 40. Everyone over age 60, especially Mexican Americans. People with a family history of glaucoma.A comprehensive dilated eye exam can reveal more risk factors, such as high eye pressure, thinness of the cornea, and abnormal optic nerve anatomy. In some people with certain combinations of these high-risk factors, medicines in the form of eyedrops reduce the risk of developing glaucoma by about half.
What are the symptoms of glaucoma?
At first, open-angle glaucoma has no symptoms. It causes no pain. Vision stays normal.
As glaucoma remains untreated, people may miss objects to the side and out of the corner of their eye. Without treatment, people with glaucoma will slowly lose their peripheral (side) vision. They seem to be looking through a tunnel. Over time, straight-ahead vision may decrease until no visual acuity remains.
Glaucoma can develop in one or both eyes.
Glaucoma is detected through a comprehensive eye exam that includes:
- Visual acuity test. This eye chart test measures how well you see at various distances.
- A tonometer measures pressure inside the eye to detect glaucoma.
- Visual field test. This test measures your side (peripheral) vision. It helps your eye care professional tell if you have lost side vision, a sign of glaucoma.
- Dilated eye exam. Drops are placed in your eyes to widen, or dilate, the pupils. Your eye care professional uses a special magnifying lens to examine your retina and optic nerve for signs of damage and other eye problems. After the exam, your close-up vision may remain blurred for several hours.
- Pachymetry. A numbing drop is applied to your eye. Your eye care professional uses an ultrasonic wave instrument to measure the thickness of your cornea.
Can glaucoma be cured?
No. There is no cure for glaucoma. Vision lost from the disease cannot be restored.
Can glaucoma be treated?
Yes. Immediate treatment for early stage, open-angle glaucoma can delay progression of the disease. That’s why early diagnosis is very important.
Glaucoma treatments include medicines, micropulse laser, SLT laser, laser trabeculoplasty, conventional surgery, or a combination of any of these. While these treatments may save remaining vision, they do not improve sight already lost from glaucoma.
Medicines for glaucoma
Medicines, in the form of eye drops or pills, are the most common early treatment for glaucoma. Some medicines cause the eye to make less fluid. Others lower pressure by helping fluid drain from the eye.
Before you begin glaucoma treatment, tell your eye care professional about other medicines you may be taking. Sometimes the drops can interfere with the way other medicines work.
Glaucoma medicines may be taken several times a day. Most people have no problems. However, some medicines can cause headaches or other side effects. For example, drops may cause stinging, burning, and redness in the eyes.
Many drugs are available to treat glaucoma. If you have problems with one medicine, tell your eye care professional. Treatment with a different dose or a new drug may be possible.
Because glaucoma often has no symptoms, people may be tempted to stop taking, or may forget to take, their medicine. You need to use the drops or pills as long as they help control your eye pressure. Regular use is very important.
Make sure your eye care professional shows you how to put the drops into your eye. See tips on using your glaucoma eyedrops.
Micropulse laser treatment for glaucoma
MicroPulse is also ideal for treating some forms of glaucoma. Traditional eye drop therapy for the management of open-angle glaucoma presents the challenges of patient compliance, high costs, and side-effects. MicroPulse laser trabeculoplasty (MLT) for glaucoma can eliminate the need for eye drop medications. MLT provides the same eye pressure lowering benefits as the traditional Selective Laser Trabeculoplasty (SLT) treatment, but is safer due to its lower energy output. MLT reduces the amount of post-treatment complications, like inflammation and eye pressure spikes, that can be seen with SLT treatments.
Laser trabeculoplasty
Laser trabeculoplasty helps fluid drain out of the eye. Your glaucoma doctor may suggest this step at any time. In many cases, you need to keep taking glaucoma drugs after this procedure.
Laser trabeculoplasty is performed in your doctor’s office or eye clinic. Before the surgery, numbing drops will be applied to your eye. As you sit facing the laser machine, your doctor will hold a special lens to your eye. A high-intensity beam of light is aimed at the lens and reflected onto the meshwork inside your eye. You may see flashes of bright green or red light. The laser makes several evenly spaced burns that stretch the drainage holes in the meshwork. This allows the fluid to drain better.
Like any surgery, laser surgery can cause side effects, such as inflammation. Your doctor may give you some drops to take home for any soreness or inflammation inside the eye. You need to make several followup visits to have your eye pressure monitored.
If you have glaucoma in both eyes, only one eye will be treated at a time. Laser treatments for each eye will be scheduled several days to several weeks apart.
Studies show that laser surgery is very good at reducing the pressure in some patients. However, its effects can wear off over time. Your doctor may suggest further treatment.
Conventional surgery
Conventional surgery makes a new opening for the fluid to leave the eye. Your doctor may suggest this treatment at any time. Conventional surgery often is done after medicines and laser surgery have failed to control pressure.
Conventional surgery is performed in an eye clinic or hospital. Before the surgery, you will be given medicine to help you relax. Your doctor will make small injections around the eye to numb it. A small piece of tissue is removed to create a new channel for the fluid to drain from the eye.
For several weeks after the surgery, you must put drops in the eye to fight infection and inflammation. These drops will be different from those you may have been using before surgery.
As with laser surgery, conventional surgery is performed on one eye at a time. Usually the operations are four to six weeks apart.
Conventional surgery is about 60 to 80 percent effective at lowering eye pressure. If the new drainage opening narrows, a second operation may be needed. Conventional surgery works best if you have not had previous eye surgery, such as a cataract operation.
In some instances, your vision may not be as good as it was before conventional surgery. Conventional surgery can cause side effects, including cataract, problems with the cornea, and inflammation or infection inside the eye. The buildup of fluid in the back of the eye may cause some patients to see shadows in their vision. If you have any of these problems, tell your doctor so a treatment plan can be developed.
What are some other forms of glaucoma?
Open-angle glaucoma is the most common form. Some people have other types of the disease.
In low-tension or normal-tension glaucoma, optic nerve damage and narrowed side vision occur in people with normal eye pressure. Lowering eye pressure at least 30 percent through medicines slows the disease in some people. Glaucoma may worsen in others despite low pressures.
A comprehensive medical history is important in identifying other potential risk factors, such as low blood pressure, that contribute to low-tension glaucoma. If no risk factors are identified, the treatment options for low-tension glaucoma are the same as for open-angle glaucoma.
In angle-closure glaucoma, the fluid at the front of the eye cannot reach the angle and leave the eye. The angle gets blocked by part of the iris. People with this type of glaucoma have a sudden increase in eye pressure. Symptoms include severe pain and nausea, as well as redness of the eye and blurred vision. If you have these symptoms, you need to seek treatment immediately. This is a medical emergency. If your doctor is unavailable, go to the nearest hospital or clinic. Without treatment to improve the flow of fluid, the eye can become blind in as few as one or two days. Usually, prompt laser surgery and medicines can clear the blockage and protect sight.
In congenital glaucoma, children are born with a defect in the angle of the eye that slows the normal drainage of fluid. These children usually have obvious symptoms, such as cloudy eyes, sensitivity to light, and excessive tearing. Conventional surgery typically is the suggested treatment, because medicines may have unknown effects in infants and be difficult to administer. Surgery is safe and effective. If surgery is done promptly, these children usually have an excellent chance of having good vision.
Secondary glaucomas can develop as complications of other medical conditions. These types of glaucomas are sometimes associated with eye surgery or advanced cataracts, eye injuries, certain eye tumors, or uveitis (eye inflammation). Pigmentary glaucoma occurs when pigment from the iris flakes off and blocks the meshwork, slowing fluid drainage. A severe form, called neovascular glaucoma, is linked to diabetes. Corticosteroid drugs used to treat eye inflammations and other diseases can trigger glaucoma in some people. Treatment includes medicines, laser surgery, or conventional surgery.
What can I do if I already have lost some vision from glaucoma?
If you have lost some sight from glaucoma, ask your eye care professional about low vision services and devices that may help you make the most of your remaining vision. Ask for a referral to a specialist in low vision. Many community organizations and agencies offer information about low vision counseling, training, and other special services for people with visual impairments. A nearby school of medicine or optometry may provide low vision services.
What research is being done?
Through studies in the laboratory and with patients, the National Eye Institute is seeking better ways to detect, treat, and prevent vision loss in people with glaucoma. For example, researchers have discovered genes that could help explain how glaucoma damages the eye.
The NEI also is supporting studies to learn more about who is likely to get glaucoma, when to treat people with increased pressure, and which treatment to use first.
What can I do to protect my vision?
If you are being treated for glaucoma, be sure to take your glaucoma medicine every day. See your eye care professional regularly.
You also can help protect the vision of family members and friends who may be at high risk for glaucoma–African Americans over age 40; everyone over age 60, especially Mexican Americans; and people with a family history of the disease. Encourage them to have a comprehensive dilated eye exam at least once every two years. Remember: Lowering eye pressure in glaucoma’s early stages slows progression of the disease and helps save vision.
Medicare covers an annual comprehensive dilated eye exam for some people at high risk for glaucoma. These people include those with diabetes, those with a family history of glaucoma, and African Americans age 50 and older.
What should I ask my eye care professional?
You can protect yourself against vision loss by working in partnership with your eye care professional. Ask questions and get the information you need to take care of yourself and your family.
What are some questions to ask?
About my eye disease or disorder
What is my diagnosis? What caused my condition? Can my condition be treated? How will this condition affect my vision now and in the future? Should I watch for any particular symptoms and notify you if they occur? Should I make any lifestyle changes? About my treatment
What is the treatment for my condition? When will the treatment start and how long will it last? What are the benefits of this treatment and how successful is it? What are the risks and side effects associated with this treatment? Are there foods, drugs, or activities I should avoid while I’m on this treatment? If my treatment includes taking medicine, what should I do if I miss a dose? Are other treatments available?
About my tests…
What kinds of tests will I have? What can I expect to find out from these tests? When will I know the results? Do I have to do anything special to prepare for any of the tests? Do these tests have any side effects or risks? Will I need more tests later?
Other suggestions
If you don’t understand your eye care professional’s responses, ask questions until you do understand. Take notes or get a friend or family member to take notes for you. Or, bring a tape recorder to help you remember the discussion. Ask your eye care professional to write down his or her instructions to you. Ask your eye care professional for printed material about your condition. If you still have trouble understanding your eye care professional’s answers, ask where you can go for more information. Other members of your health care team, such as nurses and pharmacists, can be good sources of information. Talk to them, too. Today, patients take an active role in their health care. Be an active patient about your eye care.
How should I use my glaucoma eyedrops?
If eyedrops have been prescribed for treating your glaucoma, you need to use them properly and as instructed by your eye care professional. Proper use of your glaucoma medication can improve the medicine’s effectiveness and reduce your risk of side effects.
To properly apply your eyedrops, follow these steps:
First, wash your hands. Hold the bottle upside down. Tilt your head back. Hold the bottle in one hand and place it as close as possible to the eye. With the other hand, pull down your lower eyelid. This forms a pocket. Place the prescribed number of drops into the lower eyelid pocket. If you are using more than one eyedrop, be sure to wait at least five minutes before applying the second eyedrop. Close your eye OR press the lower lid lightly with your finger for at least one minute. Either of these steps keeps the drops in the eye and helps prevent the drops from draining into the tear duct, which can increase your risk of side effects.
Also see a “Human Eye” animation
Much of this information courtesy of the National Eye Institute