Ocular histoplasmosis
A patient’s guide to ocular histoplasmosis What is histoplasmosis? Histoplasmosis is a disease caused when airborne spores of the fungus […]
Ocular histoplasmosis
A patient’s guide to ocular histoplasmosis What is histoplasmosis? Histoplasmosis is a disease caused when airborne spores of the fungus […]
A patient’s guide to ocular histoplasmosis
What is histoplasmosis?
Histoplasmosis is a disease caused when airborne spores of the fungus Histoplasma capsulatum are inhaled into the lungs, the primary infection site. This microscopic fungus, which is found throughout the world in river valleys and soil where bird or bat droppings accumulate, is released into the air when soil is disturbed by plowing fields, sweeping chicken coops, or digging holes.
Histoplasmosis, even mild cases, can cause a serious eye disease called ocular histoplasmosis syndrome (OHS), a leading cause of vision loss in Americans ages 20 to 40.
Ocular histoplasmosis syndrome?
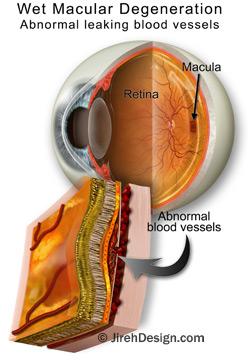
Scientists believe that Histoplasma capsulatum (histo) spores spread from the lungs to the eye, lodging in the choroid, a layer of blood vessels that provides blood and nutrients to the retina. The retina is the light-sensitive layer of tissue that lines the back of the eye. Scientists have not yet been able to detect any trace of the histo fungus in the eyes of patients with ocular histoplasmosis syndrome. Nevertheless, there is good reason to suspect the histo organism as the cause of OHS.
How does OHS develop?
OHS develops when fragile, abnormal blood vessels grow underneath the retina. These abnormal blood vessels form a lesion known as choroidal neovascularization (CNVM). If left untreated, the CNV lesion can turn into scar tissue and replace the normal retinal tissue in the macula. The macula is the central part of the retina that provides the sharp, central vision that allows us to read a newspaper or drive a car. When this scar tissue forms, visual messages from the retina to the brain are affected, and vision loss results.
Visual acuity is also impaired when these abnormal blood vessels leak fluid and blood into the macula. If these abnormal blood vessels grow toward the center of the macula, they may affect a tiny depression called the fovea. The fovea is the region of the retina with the highest concentration of special retinal nerve cells, called cones, that produce sharp, daytime vision. Damage to the fovea and the cones can severely impair, and even destroy, this straight-ahead vision. Early treatment of OHS is essential; if the abnormal blood vessels have affected the fovea, controlling the disease will be more difficult. Since OHS rarely affects side, or peripheral vision, the disease does not cause total blindness.
What are the symptoms of OHS?
OHS usually has no symptoms in its early stages; the initial OHS infection usually subsides without the need for treatment. This is true for other histo infections; in fact, often the only evidence that the inflammation ever occurred are tiny scars called “histo spots,” which remain at the infection sites. Histo spots do not generally affect vision, but for reasons that are still not well understood, they can result in complications years–sometimes even decades–after the original eye infection. Histo spots have been associated with the growth of the abnormal blood vessels underneath the retina.
In later stages, OHS symptoms may appear if the abnormal blood vessels cause changes in vision. For example, straight lines may appear crooked or wavy, or a blind spot may appear in the field of vision. Because these symptoms indicate that OHS has already progressed enough to affect vision, anyone who has been exposed to histoplasmosis and perceives even slight changes in vision should consult an eye care professional.
Who is at risk for OHS?
Although only a tiny fraction of the people infected with the histo fungus ever develops OHS, any person who has had histoplasmosis should be alert for any changes in vision similar to those described above. Studies have shown the OHS patients usually test positive for previous exposure to histoplasmosis.
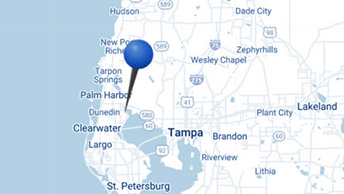
In the United States, the highest incidence of histoplasmosis occurs in a region often referred to as the “Histo Belt,” where up to 90 percent of the adult population has been infected by histoplasmosis. This region includes all of Arkansas, Kentucky, Missouri, Tennessee, and West Virginia as well as large portions of Alabama, Illinois, Indiana, Iowa, Kansas, Louisiana, Maryland, Mississippi, Nebraska, Ohio, Oklahoma, Texas, and Virginia. Since most cases of histoplasmosis are undiagnosed, anyone who has ever lived in an area known to have a high rate of histoplasmosis should consider having their eyes examined for histo spots.
How is OHS diagnosed?
An eye care professional will usually diagnose OHS if a careful eye examination reveals two conditions: (1) The presence of histo spots, which indicate previous exposure to the histo fungus spores; and (2) Swelling of the retina, which signals the growth of new, abnormal blood vessels. To confirm the diagnosis, a dilated eye examination must be performed. This means that the pupils are enlarged temporarily with special drops, allowing the eye care professional to better examine the retina.
If fluid, blood, or abnormal blood vessels are present, an eye care professional may want to perform a diagnostic procedure called fluorescein angiography. In this procedure, a dye, injected into the patient’s arm, travels to the blood vessels of the retina. The dye allows a better view of the CNVM lesion, and photographs can document the location and extent to which it has spread. Particular attention is paid to how close the abnormal blood vessels are to the fovea.
How is OHS treated?
The use of anti-VEGF drugs may be successful in treating OHS that has leaking CNVM lesions, but as of this writing, anti-VEGFs are not FDA-approved for the treatment of CNVM secondary to OHS. Click here to watch an Avastin injection animation
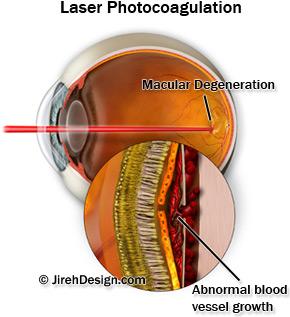
The treatment for OHS is a form of laser surgery called photocoagulation. A small, powerful beam of light destroys the fragile, abnormal blood vessels, as well as a small amount of the overlying retinal tissue. Although the destruction of retinal tissue during the procedure can itself cause some loss of vision, this is done in the hope of protecting the fovea and preserving the finely-tuned vision it provides.
How effective is laser surgery?
Controlled clinical trials, sponsored by the National Eye Institute, have shown that photocoagulation can reduce future vision loss from OHS by more than half. The treatment is most effective when:
- The CNV has not grown into the center of the fovea, where it can affect vision.
- The eye care professional is able to identify and destroy the entire area of CNV.
Does laser surgery restore lost vision?
Laser photocoagulation usually does not restore lost vision. However, it does reduce the chance of further CNV growth and any resulting vision loss.
Does laser surgery cure OHS?
No. OHS cannot be cured. Once contracted, OHS remains a threat to a person’s sight for their lifetime.
People with OHS who experience one bout of abnormal blood vessel growth may have recurrent CNV. Each recurrence can damage vision and may require additional laser therapy. It is crucial to detect and treat OHS as early as possible before it causes significant visual impairment.
Is there a simple way to check for signs of OHS damage to the macula?
Yes. A person can check for signs of damage to the macula by looking at a printed pattern called an Amsler grid. If the macula has been damaged, the vertical and horizontal lines of the grid may appear curved, or a blank spot may seem to appear.
Many eye care professionals advise patients who have received treatment for OHS, as well as those with histo spots, to check their vision daily with the Amsler grid one eye at a time. Patients with OHS in one eye are likely to develop it in the other.
What help is available for people who have already lost significant vision from OHS?
Scientists and engineers have developed many useful devices to help people with severe visual impairment in both eyes. These devices, called low vision aids, use special lenses or electronics to create enlarged visual images. An eye care professional can suggest sources that provide information on counseling, training, and special services for people with low vision. Many organizations for people who are blind also serve those with low vision.
What research is being conducted on the ocular histoplasmosis syndrome?
The National Eye Institute (NEI) supports research aimed at learning more about the relationship between histoplasmosis and OHS and how to treat OHS effectively. One such multicenter clinical study is called the Submacular Surgery Trials (SST). This clinical study is examining whether CNV in the fovea, which cannot be treated by laser photocoagulation, can be successfully removed through traditional surgery. Patients with OHS who would like to receive more information about the Submacular Surgery Trials should call the SST Chairman’s Office toll-free at 1-888-554-0412.
Information on systemic histoplasmosis can be obtained from:
The National Institute of Allergy and Infectious Diseases (NIAID)
The National Institutes of Health
Building 31, Room 7A50
31 Center Drive, MSC 2520
Bethesda, MD, 20892-2520
Telephone: 301-496-5717
Website: http://www.niaid.nih.gov
Courtesy of the National Eye Institute More information on OHS: https://jackiehendrix.wordpress.com/presumed-ocular-histoplasmosis/